70Y old suffering from Neck pain and back pain. (CKD)
This is the case of a 70-year-old male, resident of Tirumalagiri, and Farmer by occupation. The following history was taken with the patient in person. The patient was explained about confidentiality and written consent was taken to create the following case report.
This case report aims to record the patient's journey.
CHIEF COMPLAINTS:-
-Neck pain and Back pain since 10 days.
History of present illness:-
History of past illness:-
The patient has DM since 24 years and HTN since 10 years.
The patient does not have any history of TB, Epilepsy, and asthma.
Surgical history
Patient was apparently asymptomatic 8 years ago. Afterwhich the patient developed stomach pain which was later diagnosed to be cholelithiasis. The patient had undergone cholectomy. Later it was also found that the patient has CKD.
The patient has been undergoing dialysis since 4 months, with a frequency of 2-3 times per week.
The patient has undergone blood transfusion three months back.
Personal history:-
Water intake:- half a litre per day
Appetite:- reduced
Diet:- mixed
Bowel movement:- normal
Bladder movement:- normal
Alcohol:- occational consumtion for thirty years.
Smoking:- nil
Addiction:- nil
Allergies:- nil
Exercise status:- moderate
FAMILY HISTORY:-
- not significant.
PHYSICAL EXAMINATION:-
GENERAL EXAMINATION:-
The examination was conducted at a well lit and well ventilated room. The patient was conscious, cooperative and coherent.
Moderately built
Afebrile
No Palor
No Icterus
No Cyanosis
No Clubbing
No Pedal edema
No Significant lymphadenopathy
CLINICAL PICTURES:-
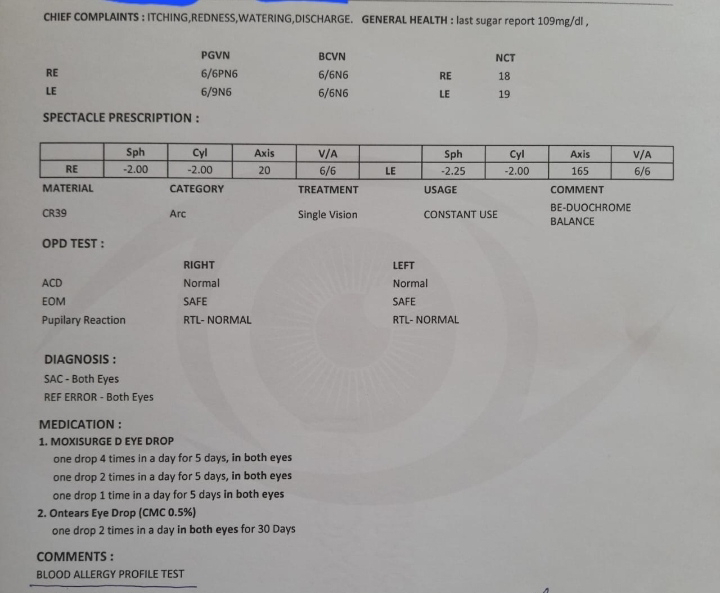
REPORTS:-







Comments
Post a Comment