My experiences with general cellular and neural cellular pathology in a case based blended learning ecosystem's CBBLE
CBBLE PaJR participatory learning action research disclaimer
NOTE: THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS/HER GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS INTENDING TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT.- uncontrolled movements in fingers and toes since 3-4 years.
- Inability to talk properly since 3 years
- Difficulty in swallowing since 2 years
- Urinary incontinence
https://96sanjanapalakodeti.blogspot.com/2022/09/53f-with-uncontrolled-hand-movements.html
After obatining the results of the neurological examination, we had reached to the conclusion that the patients, especially the man, were displaying cerebellar signs.
While interacting with the patients, I felt a mixture of feelings which till date I am not able to accurately decipher. I was awed at the tenacity of these patients, who had traveled more than 2000 kms just to receive treatment. I also remember feeling intrigued and a little upset because of their unfortunate circumstance that they were suffering from. It turns out that they weren't the only ones that had these symptoms. Their maternal grandfather, mother, and 2 maternal aunts had suffered from similar complaints at different degrees.
- Maternal Grandfather: When the patient (woman) was 5 yrs old, she witnessed his whole body 'shaking' and he fell down. After this he was bedridden and passed away.
- Mother: Had similar symptoms (fingers and toes shaking) at 56 yrs of age. This progressed to involve full body. She also fell down often and had developed a short temper. She was bedridden for 2 months and passed away at 58.
- Aunt 1 (Mothers sister): Developed symptoms at 53 yrs of age. By 60, she had loss of speech and was bedridden.
- Aunt 2 (Mothers sister): Developed symptoms at 55 yrs of age. Now bedridden.
So a pedigree chart was made and a reknown geneticist was consulted, wherein who suggested that we test for HD, SCA types 1, 3, and 12. 2ml EDTA blood samples of both the patients were sent for testing. After the results came, a diagnosis of Huntington's Chorea was made and a decision was made that the rest of the family members need to be counciled. The patients were later discharged after their condition was stabilised.
As a student researcher, I felt quite lucky to have this case as my entrée into what the clinical world had to offer. Needless to say, I was excited and had taken histories of some extra-ordinary cases, some of which taught me that being a doctor is more than just treating a disease. I shall describe one such case which has, like the first case, left an indelible impression on my view point of handling clinical cases.
Case Link:-
https://amilidutta137.blogspot.com/2022/12/17f-suffering-from-pcod.html
In this case, I had taken the patient's history over telephone. The 17 year old female patient presented with chief complaints of:-
- Hypomenorrhea since the last 7-8 months.
- Severe acne breakouts (roughly around 7-8 times in a month) as well as severe hair loss for the past 6-7 months.
- Hirsutism for the last two years.
She also mentions experiencing insomnia on a daily basis and symptoms of stress and anxiety most of the time. Her menstrual history has been erratic in my view point. With the patient starting to menstruate when she was of 10 years of age (4th grade) along with white discharge which occurs one to two days after the onset of her menstrual cycle. For the last 7 to 8 months (from October 2022), the she has noticed that there is decrease amount of blood flow for only for 3 days per month.
According to the followup on 29th November 2022, she reports that her menstrual cycle, for the first time in 4-6 months, lasted for 4 days. For the initial two days, there had been a heavy blood flow.
There was this feeling of reminisence while the patient was conveying all her problems to me. Not only did she speak about the clinical aspect of her problems but she also spoke about the psychological aspect of it. It reminded me about the troubles of being a teenager can be and being someone who has recently passed that phase, it was easier to empathasize with her. It also highlighted the fact that psychological well being is just as important to the health because there was a correlation seen with the patient's psychological health as well as the severity of the patient's symptoms.
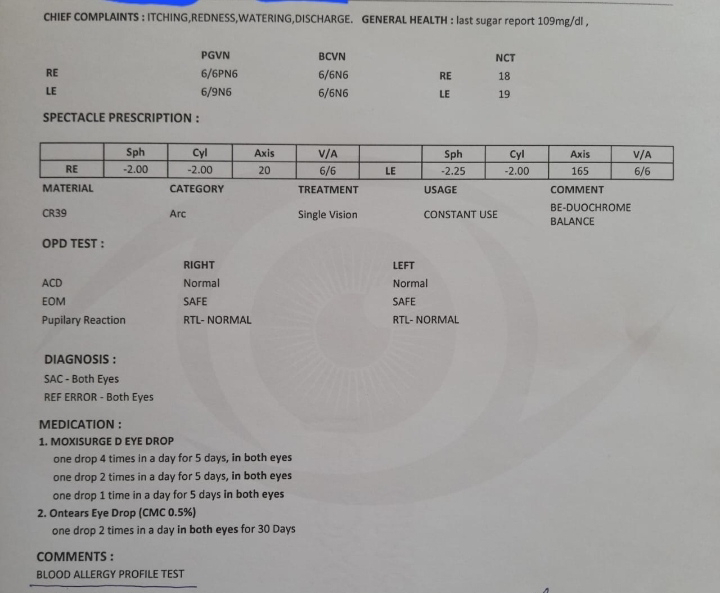
Later on, when the case report has been made, and the patient along with her family came over to her hospital. It was enlightening to be able to physically interact with them. The patient had a cheerful disposition and I was once again reminded of how vital a doctor-patient relationship is. The patient had undergone various consultations, including Dental, physiological counciling, orthopaedic, ENT as well as ophthalmic.
Dicussion of the patient's symptoms on PaJR group:-
Conversation 1:-
17/12/22, 7:58 am - Dr Rakesh Biswas HOD GM: What criteria does this patient satisfy?
17/12/22, 8:01 am - +91 99081 59666: clinically she has acne , hair loss on scalp( as told by the patient from last 2 years she has excess hair loss) and increased body and facial hair and infrequent menustration sir and Usg shows polycystic morphology of right ovary sir so accoriding to androgen excess - pcos criteria she will fit in
17/12/22, 8:08 am - Dr Rakesh Biswas HOD GM: How can you be sure that all those symptoms in her case is due to androgen excess? How can we confirm it? Also is it sufficient if the ovarian changes are seen in just one ovary?
17/12/22, 11:10 am – Dr. Arun: Acne, facial hair growth- male pattern, balding, deep voice and Increased muscle mass are the features of Hirsutism and the most common cause of Hirsutism is PCOS, almost about 75% and the next most common being idiopathic.
There is nothing about the patients dietary habits and her mental status regarding this whole weight gain and facial hair.
Because patients with PCOS are actually in a loop
Depression ( cause-young female with weight gain and facial hair)-->bingeeating--> Obesity-->increased insulin resistance --> anovulation--> no progesterone -->increased LH--> hirsutism--> depression
17/12/22, 11:15 am - Dr. Arun Yes sir.... Even if one ovary has small follicles of 2-9mm size and are more than 20, it is sufficient to provide a diagnosis of polycystic ovarian disease.
17/12/22, 11:38 am - Dr Rakesh Biswas HOD GM: @Amili Can you clarify some of the issues in your patient queried by your senior @919550434519 ?
17/12/22, 11:39 am - Dr Rakesh Biswas HOD GM: Already done. Show them the recent reports. Check if they are already available in the case report link provided by @Amili above
17/12/22, 11:40 am - Dr Rakesh Biswas HOD GM: Reference link with quote?
17/12/22, 11:42 am - Dr Rakesh Biswas HOD GM: Scientifically how was it proved that most common cause 75% of hirsutism is PCOS and did @Amili mention anything about hirsutism? What is the difference between physiological and pathological hirsutism?
17/12/22, 11:51 am - Dr. Arun: @Amili didn't mention about Hirsutism but she has mentioned all the features of Hirsutism which are seen in PCOS sir.
Hirsutism is pathological sir seen most commonly in young females who have attained puberty and male pattern- hair growth is seen in parts dependent on androgens for hairgrowth like beard and moustache
17/12/22, 11:51 am - Dr. Arun: https://www.ncbi.nlm.nih.gov/books/NBK470417/#:~:text=Moderate%20hirsutism%20can%20be%20observed,cessation%20of%20ovarian%20estrogen%20production).
17/12/22, 11:53 am - Amili: With regards to her mental status:- "She has been going for therapy for the last 4 years (roughly in the year 2018), with a frequency of once or twice in a month. " As with regards to growth of facial hair, this has been a problem since the year 2020 till today. "On July 2022, The patient has suffered from a COVID infection." Her weight from 8th grade till the time she was affected with COVID, according to the patient, was ranging around 61-63 kg. When she recovered from the infection, her weight till date is 57 kg. The patient did mention facing difficulty in losing weight despite exercising. As of her appetite, it has been reduced till date roughly since the year 2018.
- The patient's accessibility to the doctor has drastically improved as she can discuss any doubts or problems she could be having freely, and expect an quick as well as a reliable response.
- Discussions, lab reports and clinical images on the PaJR group can be later on complied and used for further research.
- Academic
discussions related to the patient’s condition with the presence of the
patient’s advocate can be overwhelming and confusing to the patient.
- Due to the adequate resources as well as properly documented symptoms, investigation reports, as well as case reports, the information could be effectively used for research.
- Improvises on the spectrum of clinical learning objectives for the medical students as they can discuss the pathogenesis and etiology of the problem with the professor and doctors on the platform.
Threats:-
- Lack of active participation of the group members.
A 28 year old female, farmer by occupation, presented with chief complaints of pain and weakness in the lower back region, right upper limb and right lower limb for 8 years.
Eight years ago, while she was drawing water from the well, she suddenly experienced pain similar to that of a muscle pull in the region of her right lower back which was of sudden onset, progressive, dragging type which gradually spread from her right lower back region, then to her right upper limb and her right lower limb. She experiences the pain with more intensity on the right arm than the left arm and then afterwards spreading to the right leg posterio-laterally. It is correlating with the onset of weakness.
Spectrum of illness over the course of eight years:-
Initially, for the period of the first five years, the pain has been increasing gradually after an interval of four to five months. With the daily activities being taken into consideration, the pain increases whenever the patient performs daily chores that involve sitting and also when she wakes up in the morning. And for the next three years, the patient reports that the severity of the pain has increased, with the pain in the joints as well. (elbow joint, joints at the phalanges, knee joint and hip joint). She experiences sensory abnormalities such as reduced sensations in the sole of her foot for the last three years, and frequent cramping of her right foot, accompanied with frequent episodes of tingling in her right lower limb.
Negative History:-
There was no history of swelling, skin changes , rash , difficulty in breathing, fasciculations of the muscles, involuntary movements, no dysphonia/hypophonia, spillage of food from the mouth, diaphoresis or palpitations, fever or vomiting.
Neurological Examination:-
All higher mental functions are intact. No abnormalities found in cranial nerve examination. Motor examination revealed hypotonia and mild atrophy of the biceps brachii and brachialis with inability to flex the right elbow joint as well as unable to perform internal rotation at the right shoulder joint and adduction of the right arm. Deep tendon reflexes were absent on the right biceps and supinator. Hyporeflexia noted on the right knee and the right plantar reflex was absent. Reflexes on the left side were normal. No distal weakness was observed. No objective evidence of sensory deficits was noted on both upper and lower limbs.
Musculoskeletal examination:-
At the time of examination, the tenderness was more restricted to the joints of the right upper limb. The tenderness present on the elbow joint was more on the right side than to the left. The squeeze test was positive on the 2nd, 3rd and 4th proximal interphalangeal joints on the right hand as well as on the 3rd and 4th proximal interphalangeal joints, 2nd and 3rd distal interphalangeal joints. Squeeze test was negative in other joints. No restriction of movement was noted.
Investigations:-
- The MRI scan of the brain revealed a few T2 / FLAIR hyperintense lesions on the right side which are oriented perpendicular to the ventricles.
- The laboratory investigations revealed that the ESR was elevated (25mm/hr), CRP was negative and CK was within normal ranges (147 IU/L).
- The NCS investigation was done with the exception of the musculocutaneous nerve and sciatic nerve. The report for both the motor as well as the sensory nerve conduction was normal.
- Needle EMG, Serum protein electrophoresis and re-investigation of the NCS couldn’t be performed due to technical limitations of the PaJR group as well as financial limitations of the patient.
Thus the patient was given a provisional diagnosis of Multifocal Motor Neuropathy and treatment regimen was started with tablet Prednisolone 10mg and Naproxene 250mg.
Academic discussion:-
This case depicts the clinical progression as well as the typical signs and symptoms that a patient of Multifocal Motor Neuropathy would display.
Multifocal motor neuropathy (MMN) is an acquired, chronic, immune-mediated demyelinating neuropathy. It is a progressive disease, which predominantly starts off as distal extremity weakness without any loss of sensation. There is an asymmetric involvement of two or more peripheral nerves without signs of upper motor neuron lesion. [1]
The incidence of this disease is with a frequency of 1-2/100 000 worldwide, with the reported prevalence of MMN is 0.65 in Austria [2] and 0.29 in Japan per 100,000 people [3]. Furthermore, MMN commonly affects men more than women with a ratio of 3:1 [1].
Most of the research articles suggest that Anti-Ganglioside Antibodies play a major role in the pathophysiology of this disease. These antibodies are present in greater concentration in the peripheral motor nerves (specifically around the nodes of Ranvier) compared to the sensory nerves. Although, the role of these antibodies GM1 isn’t fully known, they are thought to be responsible for the maintenance of tight junctions in the paranodal areas, stabilize and cluster the ion channels around the node of Ranvier, which are inturn important for the propagation of action potential. Disruption of these ion channels would lead to decreased propagation of action potential, resulting in the formation of a conduction block. This conduction block would lead to decreased conduction velocity, which can be detected on the electrophysiologic studies such as needle EMG, NCS.[4][5]
However, Anti-GM1 antibodies are not present in all cases of MMN. Patients falling in this category, may either have low undetectable titers of anti-GM1 or have different antibodies present that are directed against different antigens. [4][5] Also, these antibodies are not specific for MMN and are also seen in acute motor axonal neuropathy (AMAN) variant of Guillain-Barre syndrome, but their presence supports the diagnosis.[6]
The clinical characteristics remain the same irrespective of the presence of Anti-GM1 antibodies.[6]
In 2010, the European Federation of Neurological Societies (EFNS) and Peripheral Nerve Society (PNS) Task Force revised the following diagnostic criteria to help in the diagnosis of MMN.[7]
Core Criteria (both must be present)
- Slowly progressive, focal, asymmetric limb weakness, that is, motor involvement in the motor nerve distribution of at least two nerves, for at least 1 month (usually more than 6 months). If symptoms and signs are present only in the distribution of one nerve, only a possible diagnosis can be made.
- No objective sensory abnormalities except for minor vibration sense abnormalities in the lower limbs.[7]
- Predominant upper limb involvement[7]
- Decreased or absent tendon reflexes in the affected limb
- Absence of cranial nerve involvement
- Cramps and fasciculations in the affected limb
- Response to immunomodulatory treatment[7]
Exclusion Criteria
- Upper motor neuron signs
- Marked bulbar involvement
- Sensory impairment more marked than minor vibration loss in the lower limbs
- Diffuse symmetric weakness during the initial weeks[7]
Correlation with the patient:-
As mentioned in the case report, the symptoms reported by the patient are over 8 years, indicating that the condition was slowly progressive by nature. There was no cranial nerve involvement or bulbar involvement.
Our patient displays pain as well as weakness predominantly on the right side of both upper and lower limbs, with decreased tendon reflexes more apparent on the right upper and lower limbs. Deep tendon reflexes were absent on the right biceps and supinator, normal right tricep reflex with hyporeflexia on the right knee and the right plantar reflex was absent.[10] Reflexes on the left side were normal. No distal weakness was observed. However, instead of distal weakness, our patient had proximal weakness and there were no sensory deficits or fasciculations noted on both right and left side of the upper and lower limbs.[9]
There have been some similarities that were observed in our patient to that of the one cited in a case report by Parry GJ.[9] The patient, although male, had fasciculations developing in his right forearm with no sensory deficits. Over a period of 10 years, this has gradually progressed to weakness on the shoulder region and later developed atrophy especially on the spinati, deltoid and biceps (Our patient has mild atrophy on the Biceps brachii and brachialis). There is a possibility of sensory symptoms developing for our patient, as in the case report [9], 10 years after the onset of the initial motor symptom, intermittent paresthesias in the right thumb and index finger was observed.
Based on the results of the physical examination as well as the limited data of the conducted investigations, the probable diagnosis of MMN fits diagnostic criteria revised by the European Federation of Neurological Societies (EFNS) and Peripheral Nerve Society (PNS) Task Force.
Complications:-
Multifocal motor neuropathy is rarely fatal due to the sparing of cranial and respiratory muscles. Most complications are treatment-related.
- IVIG may cause thromboembolic events (myocardial infarctions, stroke, or deep venous thrombosis), renal failure, anaphylactic reactions, aseptic meningitis, and rarely, transfusion-related acute lung injury.
- Cyclophosphamide may cause bone marrow suppression, hemorrhagic cystitis, and interstitial pneumonitis.
Initially, the consultation was done via telecommunication as the patient resided far away from the hospital. First, the patient’s history has been taken and the case report has been prepared by one of the PaJR volunteers. At the same time, the patient as well as the patient’s advocate were informed about what the PaJR initiative entails and the consent has been taken. After which, the PaJR group was created on whatsapp, which included doctors and medical students to discuss the etiopathogenesis of the condition. Here, the patient’s diet, medication and the progression of the condition was being monitored and discussed on a daily basis through de-identified images. If the patient has any doubts or concerns regarding her condition, those would be instantly clarified by the participants of the group. In order to further examine the condition closely and effectively, the patient as well as her advocate were encouraged to come to the hospital. CNS examination, lab investigations, MRI scan were performed however some of the investigations remained incomplete due to the financial constraints of the patient. Below is the SWOT analysis of the situation:-
Strengths:-
- The patient’s doubts as well as concerns were effectively and immediately taken care of by the group participants. This enables the patient to avoid feeling more distressed than she would be thereby getting a platform to freely express and feel temporarily relieved.
- The discussions taking place in the PaJR group effectively compile the symptoms, the resource material related to explaining these symptoms, any reports of any investigations done as well as the case reports in one place, making it easier to analyze the progression of the condition.
- The need of having the patient to travel to the hospital numerous times only for follow ups of the condition has been eliminated, thereby preserving the patient’s time, and energy.
Weakness:-
- Since the patient resides far away, there was a language barrier between the patient and the doctor in charge.
- Hesitancy of the patient to share de-identified details on the group.
- Academic discussions related to the patient’s condition with the presence of the patient’s advocate can be overwhelming and confusing to the patient.
- Due to lack of resources, technical difficulties on the side of the PaJR team, as well as time constraints and financial difficulties of the patient, some of the investigations remained incomplete, which led to the case to remain incomplete and the subsequent treatment could not be discussed.
Opportunities:-
- Due to the adequate resources as well as properly documented symptoms, investigation reports, as well as case reports, the information could be effectively used for research.
- It provides a platform for medical students to be exposed to cases which they could relate with their existing theoretical knowledge.
Threats:-
- Even if the case is completed and the provincial diagnosis was reached, the failure to obtain expensive drugs such as IVIG for the treatment could otherwise create a sense of despair and distress to the patient.
- Lack of active participation of the group members.
- Multiple inputs with regards to the etiology as well as the probable diagnosis may lead to confusion.
1.
Jusufović E, Sinanović O, Zukić S, Burina A, Džinić Jusufović Z, Šakić A. MULTIFOCAL MOTOR NEUROPATHY: CASE REPORTS. Acta Clin Croat. 2018 Sep;57(3):581-587. doi: 10.20471/acc.2018.57.03.23. PMID: 31168193; PMCID: PMC6536289.
2.
Löscher WN,Oberreiter EM,Erdler M,Quasthoff S,Culea V,Berek K,Embacher N,Grinzinger S,Hess I,Höger FS,Horlings CGC,Huemer M,Jecel J,Kleindienst W,Laich E,Müller P,Oel D,Örtl W,Lenzenweger E,Rath J,Stadler K,Stieglbauer K,Thaler-Wolf C,Wanschitz J,Zimprich F,Cetin H,Topakian R, Multifocal motor neuropathy in Austria: a nationwide survey of clinical features and response to treatment. Journal of neurology. 2018 Dec; [PubMed PMID: 30259176]
3.
Kamata A,Muramatsu K,Sawaura N,Makioka N,Ogata T,Kuwashima M,Arakawa H, Demyelinating neuropathy in a 6-year-old girl with autism spectrum disorder. Pediatrics international : official journal of the Japan Pediatric Society. 2017 Aug; [PubMed PMID: 28804976]
4.
Léger JM, Guimarães-Costa R, Iancu Ferfoglia R. The pathogenesis of multifocal motor neuropathy and an update on current management options. Ther Adv Neurol Disord. 2015 May;8(3):109-22. doi: 10.1177/1756285615575269. PMID: 25941538; PMCID: PMC4409549.
5.
Miyashiro A,Matsui N,Shimatani Y,Nodera H,Izumi Y,Kuwabara S,Imai T,Baba M,Komori T,Sonoo M,Mezaki T,Kawamata J,Hitomi T,Kawamata J,Hitomi T,Kohara N,Arimura K,Hashimoto S,Arisawa K,Kusunoki S,Kaji R, Are multifocal motor neuropathy patients underdiagnosed? An epidemiological survey in Japan. Muscle [PubMed PMID: 24741683]
6.
Lawson VH, Arnold WD. Multifocal motor neuropathy: a review of pathogenesis, diagnosis, and treatment. Neuropsychiatr Dis Treat. 2014 Apr 5;10:567-76. doi: 10.2147/NDT.S39592. PMID: 24741315; PMCID: PMC3983019.
7.
Joint Task Force of the EFNS and the PNS. European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of multifocal motor neuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society--first revision. J Peripher Nerv Syst. 2010 Dec;15(4):295-301. doi: 10.1111/j.1529-8027.2010.00290.x. PMID: 21199100.
8.
Jinka M,Chaudhry V, Treatment of multifocal motor neuropathy. Current treatment options in neurology. 2014 Feb; [PubMed PMID: 24395647]
9.
Parry GJ. AAEM case report #30: multifocal motor neuropathy. Muscle Nerve. 1996 Mar;19(3):269-76. doi: 10.1002/(SICI)1097-4598(199603)19:3<269::AID-MUS1>3.0.CO;2-B. PMID: 8606689.
10.
Vanhoutte EK, Faber CG, van Nes SI, Jacobs BC, van Doorn PA, van Koningsveld R, Cornblath DR, van der Kooi AJ, Cats EA, van den Berg LH, Notermans NC, van der Pol WL, Hermans MC, van der Beek NA, Gorson KC, Eurelings M, Engelsman J, Boot H, Meijer RJ, Lauria G, Tennant A, Merkies IS; PeriNomS Study Group. Modifying the Medical Research Council grading system through Rasch analyses. Brain. 2012 May;135(Pt 5):1639-49. doi: 10.1093/brain/awr318. Epub 2011 Dec 20. PMID: 22189568; PMCID: PMC3338921.
Comments
Post a Comment