A 48 Y old suffering from severe Abdominal Pain and Lower Back pain.
This is the case of a 48-year-old male, resident of West Bengal, and Home Maker by occupation. The following history was taken with the patient in person. The patient was explained about confidentiality and written consent was taken to create the following case report.
This case report aims to record the patient's journey.
CHIEF COMPLAINTS:-
- For the past 5 Years, the patient has reported to be suffering from the following conditions:-
A) "Gas" in the stomach
B) Severe lower back pain
C) Bloating of the abdomen
-For the past 2-3 years, the patient has reported to be experiencing:-
A) Shortness of Breath
B) Cough
- For the past 1 year, the patient has also reported to be suffering from:-
A) Dizziness
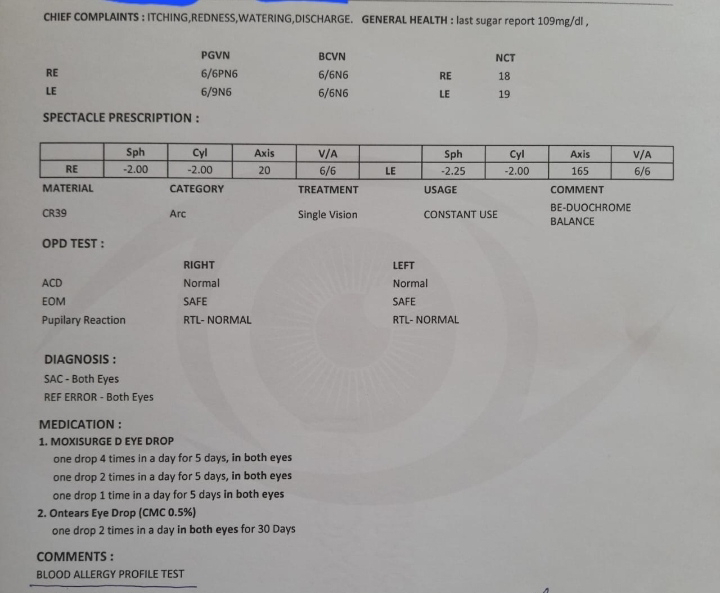
B) Eye problem (could be Hypermetropia)
History of present illness:-
The patient was a former biscuit factory owner who had retired 5 years ago due to the severe pain in the abdomen. The pain is localised in the umbilicus region as well as the Left Hypochondrium region. The patient describes this pain to be dragging. Ever since the onset of this pain began five years ago, it has become severe recently. The pain seems to increase during especially during the evening time. The patient also reports the pain to be increase while in empty stomach and before eating but the pain decreases during eating. Sometimes the patient reports that the pain increases after eating.
The patient reports to excreting stools of "Oily consistancy", with a frequency of 3-4 times a day. This frequecy would sometimes increase to 5-6 times if the abdominal pain increases or situations like acidity takes place. The patient reports to not be able to defecation completely and to be dizzy while excreting. There has been a case where he has fallen down in the toilet after excreting a 2-3 years ago. There is no change in the intensity of the abdominal pain after before and after defecation.
In addition to suffering from severe abdominal pain for five years, during the same period of time, he has reported to be suffering from Hip pain and lower back pain. The onset of this pain was from 5 years ago and the patient reports to have started from the Hip region, on both sides. The reason that the patient gives is due to his previous occupation, where he had to spend hours sitting and cutting the biscuit dough. This has then slowly spread to the lower back region. The nature of the pain, as the patient decribes, is dragging. There is no stiffness of the back and it increases while passing stool, if the abdominal pain has increased, or if the patient is asked to get up from the sitting position to a standing position. The pain, however reduces when the patient stands for sometime. The patient reports to not be able to walk with his back straight. There is no pain in his joints, however, he does mention to have a burning sensation in both the legs from knee to the sole of the foot.
For the past 2-3 years, the patient has reported to be experiencing shortness of Breath. This problem becomes apperent to the patient when he wakes up in the morning, which lasts for around 2-3 minutes. The patients also complains about suffering from wet cough. The sputum, as observed by the patient, is white and it increases when it's cold.
The patient also complains experiencing tachycardia. This increases especially during cold weather and after performing intense tasks such as lifting a heavy load. It is a constant condition, which especially occurs after the patient wakes up in the morning.
For the past 1 year, the patient has also reported to be suffering from Dizziness and Eye problem. He is unable to read small font or see anything near him properly.
History of past illness:-
The patient does not have any history of TB, HTN, DM, Epilepsy and asthma.
Personal history:-
Water intake:- reduced (1-1.5 L per day)
Appetite:- reduced (patient complains feeling full after eating small quantity of food)
Diet:- mixed (also specifically mentions having rice and spicy food three times a day. Does not consume alot of oily food and maida.)
Bowel movement:- irregular bowel movement, stools of oily consistancy with an average frequency of excreting 3-4 times a day)
Bladder movement:- Normal.
Alcohol:- used to consume 1 peg of alcohol occationally in the past, but for 5-7 years has completely stopped consumpripn of alcohol.
Smoking:- smokes 1 packet per day on a daily basis.
Allergies:- none.
Exercise status:- none
CLINICAL PICTURES:-
RADIOLOGY REPORT:-
REPORTS:-





















Comments
Post a Comment